Mpox (Monkeypox)
Mpox, commonly known as monkeypox, is a viral infection that can be transmitted between humans and animals. It belongs to the orthopoxvirus genus, which includes other notable viruses such as variola (smallpox), vaccinia, and cowpox. Monkeypox was first identified in 1958 among laboratory monkeys, and the initial human case was documented in 1970 in the Democratic Republic of Congo (DRC).
While monkeypox was predominantly found in isolated regions of central and western Africa, recent years have seen its emergence in other parts of the world, attracting significant global attention and raising concerns about a potential pandemic. Understanding monkeypox—its origins, clinical symptoms, prevention strategies, and treatment options—is essential for effectively managing and mitigating the impact of this disease.

Mpox Virus Classification
The Mpox virus is divided into two primary groups, each with distinct characteristics and varying degrees of pathogenic severity:
- Group 1 (Clade I) – Congo Basin Clade
- Characteristics: This clade is primarily found in central Africa, especially in the Democratic Republic of Congo (DRC), and is generally associated with higher pathogenicity.
- Pathogenic Severity: Clade 1 is linked to more severe symptoms and a higher incidence of complications compared to Clade 2, with a mortality rate that can exceed 10%.
- Transmission: The increased pathogenicity of this clade facilitates its spread among vulnerable populations, including children and individuals with compromised immune systems.
- Group 2 (Clade II) – West African Clade
- Characteristics: Predominantly located in West Africa, particularly Nigeria, this clade exhibits lower pathogenicity than Clade 1.
- Pathogenic Severity: Symptoms associated with Clade 2 are generally less severe, and the mortality rate is below 1%.
- Transmission: Although capable of transmission, this clade poses a reduced threat to the wider population due to its milder disease severity.
The West African Clade is further divided into two subtypes: 2a and 2b, with subtype 2b being the mutated variant identified as the cause of the recent global outbreak.

Monkeypox Transmission Methods
Mpox, also known as monkeypox, is a viral illness affecting both humans and animals, primarily spreading through direct contact with infected individuals or animals. The transmission methods can be categorized as follows:
- Animal-to-Human Transmission
- Direct Contact: The most common method of Mpox transmission occurs through direct interaction with infected animals, particularly rodents like squirrels and mice, as well as other mammals, such as monkeys. Humans can be infected by coming into contact with the blood, bodily fluids, or skin lesions of these animals.
- Consumption of Contaminated Animal Products: Eating raw or undercooked meat from infected animals poses a significant risk for virus transmission. It is advisable to ensure that meat is thoroughly cooked, especially in regions where Mpox is prevalent.
- Human-to-Human Transmission
- Direct Contact: The Mpox virus can spread through direct interaction with the skin lesions, bodily fluids, or respiratory droplets of an infected person. This can occur in various contexts, such as during medical care, handshakes, kissing, or sexual intercourse.
- Transmission Through Respiratory Droplets: The virus is transmitted via large respiratory droplets expelled from the mouth or nose of an infected individual. This mode of transmission typically requires close and intimate contact, often in face-to-face settings.
- Transmission Through Contaminated Surfaces: Mpox can also be transmitted through contact with contaminated surfaces. The virus can survive on items such as bedding, clothing, and other materials exposed to the bodily fluids or skin lesions of an infected person or animal. If a person touches these surfaces and then their mouth, nose, eyes, or any open wounds, they may risk contracting the virus. The survival duration of the virus on surfaces varies based on factors such as temperature, humidity, surface porosity, and exposure to sunlight. Generally, the virus can remain viable on surfaces for several hours to several days while still capable of causing infection.
Mpox Symptoms
Mpox, formerly known as monkeypox, presents symptoms that are similar to smallpox, though they are generally less severe. The progression of Mpox typically occurs in two distinct phases:
- Invasion Phase (Lasts 1 to 5 days)
- Fever: A sudden onset of fever, often high.
- Headache: Severe headaches can occur.
- Muscle Pain: Muscle pain, particularly in the back and legs.
- Fatigue: A general feeling of tiredness and weakness.
- Swollen Lymph Nodes: Lymphadenopathy, or swollen lymph nodes, is a key distinguishing symptom of Mpox compared to smallpox.
- Skin Lesion Occurrence Phase
- Skin Rash: Typically appears 1 to 3 days after the initial fever, starting on the face and spreading to other areas of the body, including the palms and soles.
- Lesions: The rash progresses through several distinct phases:
- Macules: Flat, discolored spots on the skin.
- Papules: Elevated, solid lesions often characterized by redness and inflammation.
- Vesicles: Small, fluid-filled blisters.
- Pustules: Deeper skin lesions containing pus.
- Crusts: Once pustules dry out, they form crusts that eventually detach.
The number of lesions can range from a few to several thousand, depending on the severity of the infection. In more severe cases, these lesions may merge, resulting in the loss of large patches of skin.
- Mucosal Lesions: Ulcers can also develop on the mucous membranes within the oral cavity as well as in the genital or anal regions.
Additional symptoms may include chills, sore throat, and cough.

Severity and Complications of Mpox
The severity of symptoms and complications associated with Mpox (formerly known as monkeypox) can vary significantly among individuals. While most cases are mild and resolve without treatment, more severe complications can occur, particularly in vulnerable populations.
Severity of the Disease:
- Mild Cases: Many individuals infected with Mpox report mild flu-like symptoms, often accompanied by a rash. These cases typically resolve within a few weeks without the need for medical intervention.
- Severe Cases: In some individuals, particularly those with compromised immune systems, pregnant women, young children, and those with pre-existing health conditions, the disease can manifest in more severe forms.
Individuals at Higher Risk for Severe Cases:
- Immunocompromised Individuals: Those with weakened immune systems, including individuals with illnesses or those taking immunosuppressive medications.
- Children Under One Year Old: This age group is particularly vulnerable.
- Individuals with Eczema: A history of eczema can increase the risk of severe symptoms.
- Pregnant Women: Pregnancy poses additional risks for complications.

- Secondary Infections: Skin lesions may become infected with bacteria, leading to serious complications if not treated.
- Pneumonia: The Mpox virus can cause respiratory issues, including pneumonia.
- Encephalitis: In rare cases, Mpox can lead to brain inflammation, known as encephalitis, which carries significant risks.
- Sepsis: This life-threatening condition is a critical response to infection that can result in organ failure.
- Eye Complications: The virus can affect the eyes, leading to conditions such as conjunctivitis, and in severe cases, vision loss.
- Scarring: Skin lesions can leave permanent scars, especially if they become infected or do not heal properly.
Risk Factors for Severe Complications
- Compromised Immune Systems: Individuals with conditions such as HIV/AIDS or those undergoing chemotherapy are at a higher risk of severe complications.
- Children: Young children are more likely to experience severe symptoms and complications from the disease.
- Pregnant Women: Expecting mothers may face complications that pose risks to both their health and that of the fetus.
Mortality
Mpox typically has a lower fatality rate compared to smallpox; however, the mortality rate can vary based on the specific virus strain and the availability of healthcare services. The Congo Basin (Central African) variant is associated with a higher mortality rate than the West African variant.
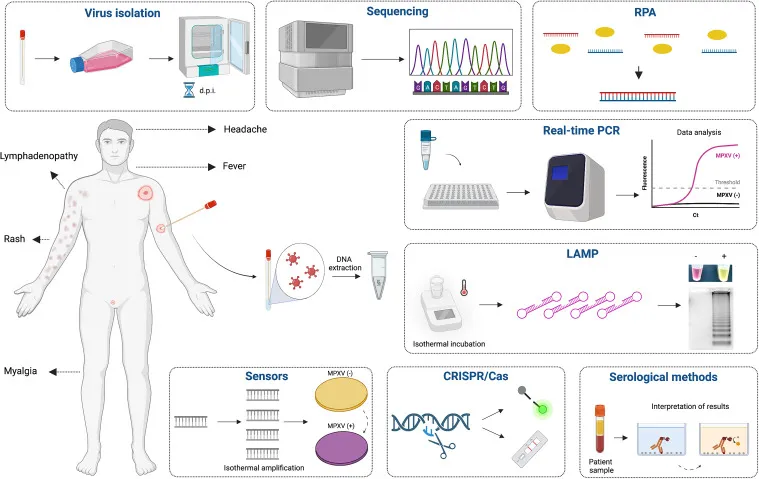
Diagnosis Methods for Mpox
Diagnosing Mpox involves a combination of clinical and laboratory methods to confirm the infection effectively:
- Clinical Diagnosis
The first step in identifying potential cases of Mpox often involves a clinical diagnosis, especially in regions where the disease is endemic or during outbreaks. Healthcare providers evaluate patients based on their symptoms, exposure history, and key indicators, including:
- Fever
- Headache
- Muscle aches
- Swollen lymph nodes
- Skin rash that progresses through various stages (flat lesions, raised bumps, blisters, pustules, and scabs)
While clinical diagnosis is vital for early detection, it has limitations. Many symptoms of Mpox overlap with those of other illnesses, such as smallpox, chickenpox, and various viral skin conditions. Therefore, clinical diagnosis should be supplemented with laboratory testing for a conclusive diagnosis.
- Laboratory Diagnosis
Laboratory testing is essential for verifying Mpox infection. Several methods can detect the virus, its components, or the immune response triggered by the infection.
- A) Polymerase Chain Reaction (PCR)
PCR is the gold standard for diagnosing Mpox due to its high sensitivity and accuracy. This technique detects viral DNA in various clinical samples, including blood, skin lesions (swabs from blisters or pustules), throat swabs, and other bodily fluids.
- Method: DNA is extracted from the sample and amplified using virus-specific primers to target sequences of the Mpox virus genome.
- Advantages: PCR can detect the virus in the early stages of infection, even at low concentrations, and can differentiate between Mpox and other orthopoxviruses, including smallpox. Results are typically available within a few hours to a day.
- Limitations: PCR requires specialized laboratory equipment, skilled personnel, and a fully equipped lab, which may be unavailable in resource-limited settings. Proper collection, management, and transportation of samples are also crucial to prevent contamination or degradation of viral DNA.
- B) Serological Tests
Serological tests identify the presence of IgM and IgG antibodies produced by the immune system in response to a Mpox infection. These tests are useful for detecting both recent and past infections, particularly when PCR testing is unavailable or when the infection has progressed beyond the stage where the virus can be detected.
- Method: Blood samples are analyzed using techniques like ELISA (Enzyme-Linked Immunosorbent Assay) or Immunofluorescence Assay (IFA) to identify specific antibodies targeting Mpox virus antigens.
- Advantages: Serological tests are generally straightforward and cost-effective, making them suitable for a wide range of laboratory settings.
- Limitations: These tests have lower sensitivity and accuracy compared to PCR during the early stages of infection, as antibodies may not yet be present. Cross-reactivity with antibodies from other orthopoxviruses can lead to false positives, and serological tests cannot differentiate between current and previous infections.
- C) Virus Isolation and Culture
Virus isolation involves growing the Mpox virus in a controlled laboratory environment using cell culture techniques. This method is primarily used in research and reference laboratories.
- Method: Clinical samples are inoculated into cell cultures that allow the Mpox virus to proliferate. Confirmation of the virus’s presence is achieved by observing specific cytopathic effects (CPE) under a microscope or through molecular methods.
- Advantages: Isolating the virus provides definitive evidence of a live virus and enables further research, including antiviral susceptibility testing and genomic sequencing.
- Limitations: This method is time-consuming, taking several days to weeks, and requires advanced biosafety facilities, posing a biohazard risk to laboratory staff.
The diagnosis of Mpox relies on a combination of clinical assessment and laboratory tests to confirm the infection and support public health measures.
Treatment and Control Methods for Monkeypox (Mpox)
Monkeypox (Mpox) is a rare but significant viral illness that requires effective strategies for prevention, management, and outbreak control. Below are the primary methods for treating and controlling this disease:
- Vaccination
Vaccination is one of the most effective ways to prevent monkeypox. Smallpox vaccines, such as the Jynneos vaccine (also known as MVA-BN), provide partial protection against Mpox and are recommended for individuals at higher risk of infection. This group includes:
- Healthcare professionals
- Individuals in close contact with infected patients
- Residents of areas where the disease is endemic
Pre-contact Prevention: Receiving the vaccine before exposure to the virus can significantly reduce the risk of contracting the disease.
Post-contact Prevention: Vaccination within four days following exposure can prevent the onset and severity of the disease, and it may reduce symptom severity for up to 14 days post-exposure.
- Quarantine and Isolation
Quarantine and isolation are crucial for effectively managing Mpox outbreaks:
- Isolation of Patients: Individuals diagnosed with Mpox must remain isolated until their skin lesions have fully healed and all symptoms have resolved. This minimizes the risk of spreading the virus. It is important to use well-ventilated spaces, wear protective clothing, and adhere to health protocols.
- Isolation of Close Contacts: Individuals who have had close contact with Mpox patients should be monitored and isolated for the duration of the virus’s incubation period, which typically lasts 21 days. This measure helps prevent the virus’s spread should any symptoms develop.
- Antiviral Treatment
Currently, there is no approved antiviral treatment specifically for Mpox; however, medications like tecovirimat (TPOXX) may be used under emergency authorization in certain cases.
- Tecovirimat: This medication helps reduce symptom severity and promotes faster recovery, particularly in severe cases or among individuals with compromised immune systems.
- Brincidofovir: This antiviral may also be used in emergency situations, although information regarding its efficacy against Mpox is limited.
- Symptomatic Treatments
Most treatments for Mpox are symptomatic, focusing on alleviating symptoms and preventing complications:
- Symptom Management: Antipyretics and pain relievers are used to control fever, pain, and discomfort.
- Hydration and Nutrition: Ensuring adequate fluid intake and proper nutrition supports faster recovery.
- Treatment of Secondary Infections: Antibiotics may be prescribed if secondary bacterial infections, such as skin infections, occur.
- Hospital Care: Severe cases may require hospitalization for specialized medical attention.
Additional Strategies for Controlling Monkeypox Outbreaks
- Education and Awareness:Educating communities and healthcare professionals about preventive strategies, recognizing the signs and symptoms of Mpox, and outlining essential actions to take in case of infection or exposure.
- Enhanced Monitoring and Reporting:Continuous surveillance of potential cases and prompt notification to health authorities are vital to prevent larger outbreaks.
- Personal and Environmental Hygiene:Following hygiene protocols, such as regular handwashing, wearing masks during patient interactions, and disinfecting potentially contaminated surfaces, is essential.
Effective management and treatment of Mpox require a multifaceted approach that includes vaccination, patient isolation, supportive care, antiviral medications, and comprehensive preventive strategies. As case numbers rise, increasing awareness and strengthening healthcare system readiness are crucial.
Principles of Personal Hygiene and Protective Measures
To prevent the spread of monkeypox, adopting personal hygiene practices and protective measures is essential:
- Avoid Contact with Infected Animals: Individuals living in or visiting endemic regions should avoid interacting with animals that could carry the monkeypox virus, particularly rodents. It is also advisable to consume only thoroughly cooked meat in these areas to minimize risk.
- Hand Hygiene: Regular handwashing with soap and water, or the use of hand sanitizers, significantly reduces the likelihood of transmission. It’s important to practice hand hygiene frequently, especially after potential exposure.
- Use of Protective Equipment: Healthcare professionals and caregivers should wear personal protective equipment (PPE) such as gloves, masks, and protective clothing when caring for infected individuals to prevent transmission.
Hypochlorous Acid: An Effective Disinfectant Against Monkeypox Virus
In the absence of specific antiviral treatments, it is critical to implement effective disinfection methods to curb the spread of the monkeypox virus. Hypochlorous acid (HOCl) has emerged as a powerful and safe disinfectant capable of destroying pathogens, including the monkeypox virus.

What is Hypochlorous Acid?
Hypochlorous acid (HOCl) is a weak acid naturally produced by the human immune system in response to infection or injury. This compound plays a vital role in the body’s innate immune defense, primarily synthesized by neutrophils, a type of white blood cell, to eliminate harmful pathogens, including bacteria, viruses, and fungi. HOCl is considered non-toxic and safe for various applications.
How Hypochlorous Acid Works Against Viruses
Hypochlorous acid acts as a potent oxidizing agent, efficiently altering the structure and functionality of viral particles. It works through several mechanisms:
- Oxidation of Viral Proteins: HOCl oxidizes the proteins found on the surface of viruses, including their coat and capsid proteins. This oxidation leads to structural changes that impair the virus’s ability to bind to and penetrate host cells.
- Disruption of Lipid Membranes: Many viruses, including the monkeypox virus, have an outer lipid membrane that protects them from the environment. Hypochlorous acid disrupts this lipid membrane, effectively inactivating the virus and preventing it from infecting host cells.
- Damage to Nucleic Acids: HOCl induces oxidative damage to the nucleic acids (DNA or RNA) of viral particles, resulting in mutations or breaks in the virus’s genetic material. This process inhibits the virus’s ability to replicate and spread.

The properties of HOCl make it an exceptionally effective broad-spectrum antiviral agent. Its rapid and efficient pathogen elimination is crucial in healthcare and public environments, where minimizing virus transmission is vital for effective infection control.
The Potential of Hypochlorous Acid Against Monkeypox Disease
Monkeypox is categorized as an enveloped virus, characterized by a lipid membrane surrounding its protein capsid and genetic material. Enveloped viruses like monkeypox are typically more susceptible to disinfectants that target lipid membranes, including hypochlorous acid (HOCl). Research shows that HOCl can effectively inactivate a range of enveloped viruses, including coronaviruses, influenza viruses, and other orthopoxviruses, such as monkeypox and smallpox.
Advantages of Using Hypochlorous Acid for Disinfection
- Broad-Spectrum Antimicrobial Action: HOCl is effective against a wide variety of pathogens, including bacteria, fungi, and viruses. This versatility makes it an ideal disinfectant for various settings.
- Safety for Humans and Animals: Unlike many conventional chemical disinfectants, HOCl is non-toxic, non-irritating, and safe for use around humans, animals, and food. It does not release harmful fumes or leave hazardous residues, making it particularly suitable for enclosed spaces.
- Eco-Friendly: Hypochlorous acid quickly decomposes into water and chloride ions, both of which are environmentally safe. Its use does not contribute to pollution or the development of antimicrobial resistance.
- Fast Acting: HOCl can neutralize pathogens rapidly, typically within seconds to minutes of exposure.
Applications in Infection Control
HOCl can be employed across various environments to help prevent the transmission of monkeypox:
- Healthcare Centers: Disinfecting frequently touched surfaces, medical equipment, and areas designated for patient care to reduce the risk of virus spread.
- Public Transportation and Public Spaces: Regularly disinfecting high-contact surfaces such as seats and handles to minimize transmission risks.
- Personal Hygiene: Hand sanitizers and disinfectant sprays containing HOCl can significantly lower the likelihood of transmission between individuals, providing an added layer of protection.
- Animal Care Centers: Disinfecting cages, tools, and surfaces in veterinary clinics and animal shelters to prevent potential zoonotic transmissions.
Conclusion
Although monkeypox is generally less severe than smallpox, it remains a significant public health concern, particularly in regions where the virus is endemic. Global initiatives focused on monitoring, preventing, and controlling monkeypox outbreaks are essential to curbing its spread. Key strategies in the fight against monkeypox include vaccination, public health interventions, and strict personal hygiene practices. Unlike smallpox, which exclusively affects humans, monkeypox can be transmitted between humans and animals, making eradication through vaccination alone impossible. Therefore, maintaining hygiene practices is crucial in preventing the emergence and spread of this disease.