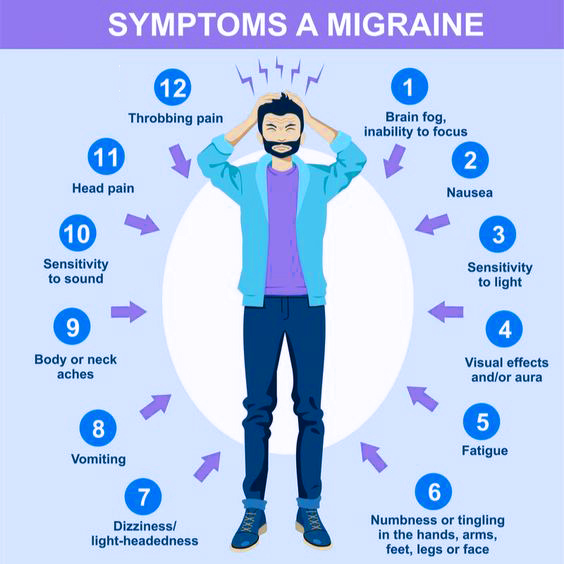
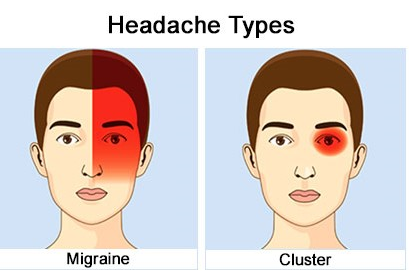
A study featured in the HEADACHE journal in 2022 demonstrated that psilocybin mushrooms effectively alleviate cluster headaches and reduce the frequency of attacks. The study underscored the positive effects of psilocybin consumption, particularly when used in conjunction with a placebo, in the treatment of chronic cluster headaches.
These treatments were provided in two sessions, spaced two weeks apart. The results, observed after two weeks, indicated that psilocybin consumption led to a greater reduction in attacks compared to the placebo. These findings highlighted the sustained and long-lasting benefits of psilocybin treatment in migraine patients.