The Gold Standard for Wound and Scar Treatment
Introduction to HOCl
Hypochlorous acid (HOCl) is synthesized within leukocytes through the interaction of chloride ions and hydrogen peroxide, facilitated by the enzyme myeloperoxidase. This compound is recognized for its stability and potent oxidizing properties, serving as a powerful antimicrobial agent deployed by the immune system to combat various pathogens, including bacteria, viruses, fungi, and even cancer cells. Notably, HOCl can penetrate bacterial biofilms, effectively eradicating them. Additionally, by providing oxygen to wounds, it significantly accelerates the healing process.

History of HOCl
In 1811, the esteemed chemist Sir Humphrey Davy, famed for his inventions such as Davy’s lamp and his discoveries of numerous chemical elements, identified hypochlorous acid as a compound produced by the human body to fight infections. Subsequently, his student, Michael Faraday, successfully isolated and produced hypochlorous acid through the process of electrolysis.
During World War I, specifically in 1914, hypochlorous acid was employed to treat injuries sustained by soldiers. HOCl was used for wound cleansing, leading to rapid recovery for those who received its benefits.

Requirements for an Ideal Wound Cleaning Solution
An effective topical treatment for wound coverage should meet several key criteria:
- Non-toxic: It should be cytotoxic-free, ensuring safety for bodily tissues.
- Minimal immune response: The solution should not provoke an immune reaction in the body.
- Pathogen reduction: It must significantly reduce pathogenic bacteria.
- Lack of bacterial resistance: The solution should remain effective against resistant strains, such as staphylococcus.
- Non-sensitizing: It should not cause skin sensitivities or allergic reactions.
- Accessibility: Easy access to the product is essential for users.
- Affordability: Cost-effective options are crucial for widespread use.

Commonly Used Antiseptics
Isopropyl alcohol, povidone-iodine (Betadine), and chlorhexidine are frequently utilized as antiseptics in dermatological, medical, and cosmetic settings. However, they come with limitations:
- Isopropyl Alcohol: While it is affordable, isopropyl alcohol can induce inflammation, has a short duration of action, lacks long-lasting antimicrobial properties, and is flammable.
- Povidone-Iodine (Betadine): It acts quickly but loses efficacy upon contact with human blood and sputum.
- Chlorhexidine: This agent is commonly used for skin antisepsis, providing strong antimicrobial effects prior to surgical procedures. However, there is a significant risk of ocular toxicity, particularly if it comes into contact with the eyes, which can lead to corneal injury and visual disturbances. This poses a considerable concern for dermatologists, plastic surgeons, and skin care specialists.
Advantages of Hypochlorous Acid (HOCl)
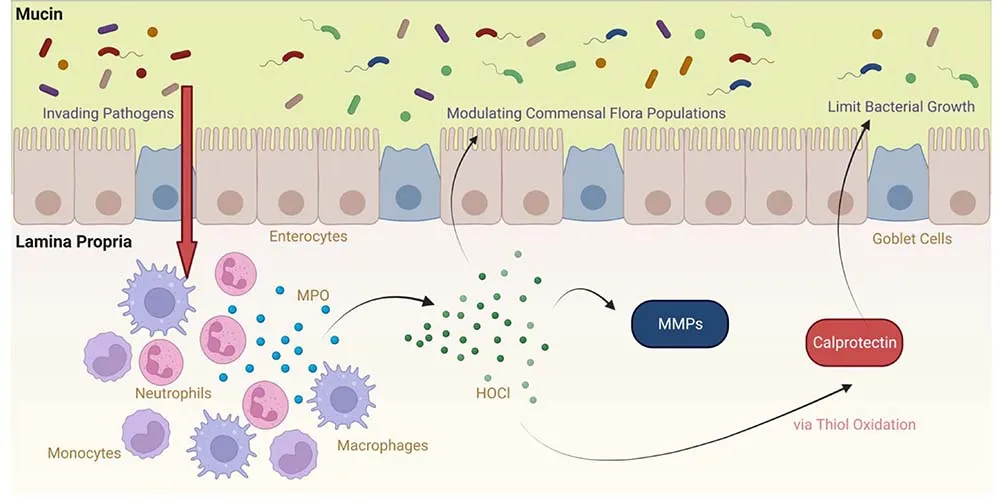
Hypochlorous acid (HOCl) stands out for its potent antimicrobial properties against a wide range of microorganisms. When skin is compromised, it creates opportunities for pathogens to invade. In response, neutrophils migrate to the site of infection, utilizing hypochlorous acid as an oxidizing agent to eliminate the intruders, effectively leveraging the body’s natural defenses.
HOCl is particularly appealing for wound care and surgical applications due to its robust efficacy and lack of microbial resistance, combined with its compatibility with human cells. It does not require adherence to COSHH (Control of Substances Hazardous to Health) regulations for storage, handling, or disposal.
Additionally, HOCl is biocompatible, posing no harm to human tissues. As a non-irritating and non-allergenic agent, it exhibits rapid antimicrobial action and strong anti-inflammatory effects, making it an optimal choice for promoting wound healing following medical and cosmetic interventions.
The Wound Healing Process
Wound healing is a complex process involving a series of interconnected biological responses, typically categorized into three distinct stages: inflammation, proliferation, and maturation (or remodeling). Each stage features a progressive change in cytokines that affect both cellular and extracellular components within the epithelium and underlying mesenchymal tissue.
It’s important to note that these phases are not strictly sequential; cell proliferation can begin before the inflammation phase has fully resolved and continues throughout the remodeling phase. Moreover, wound healing can extend beyond these primary stages, making it essential to view wound care and healing as a dynamic continuum. The long-term goal is to minimize scar formation.
Scientific studies indicate that effective skin care management before, during, and after surgery—especially during the immediate postoperative and recovery phases—can significantly impact wound healing outcomes. Therefore, diligent management of surgical wounds at each stage is vital to preventing infections, minimizing scars, and reducing the risk of additional skin complications.

The Role of Biofilm and Hypochlorous Acid (HOCl)
Biofilm formation can lead to a harmful inflammatory cycle, resulting in the prolonged presence of macrophages and neutrophils in the wound area. This disruption hampers normal wound healing and complicates antimicrobial therapy due to both biofilm presence and microbial resistance. This is where hypochlorous acid (HOCl) becomes crucial.
Even at low concentrations ranging from 0.1 to 2.8 micrograms per milliliter, HOCl demonstrates broad-spectrum antimicrobial activity. Remarkably, it can eradicate 99.99% of microorganisms in just 2 minutes at these concentrations. Moreover, when applied at higher concentrations of 200 parts per million (ppm), HOCl can eliminate 99.99999% of microorganisms. This powerful agent not only infiltrates biofilms but effectively dismantles them, significantly contributing to the success of wound healing.
Improvement of Inflammation, Itching, and Pain in Wound Care
Wounds often induce inflammatory effects characterized by pain, inflammation, and itching. These symptoms are exacerbated by immune system mediators such as histamine and prostaglandins. Hypochlorous acid (HOCl) is effective in managing these inflammatory responses, primarily by regulating mast cell activity, which has anti-inflammatory properties.
Mast cells are key components of the immune system that play a crucial role in the body’s defense against pathogens. They promote inflammation at the wound site and help prevent the spread of infections. Research has shown that HOCl stabilizes mast cell membranes, inhibiting cellular processes that trigger the release of granules containing histamine and prostaglandins, while leaving the IgE signaling pathway unaffected. This leads to significant improvements in wound size and infection control, alongside a substantial reduction in inflammatory symptoms.
The Impact of Itchiness and Pain on Wound Care
Itchiness and related pain are critical considerations in effective wound care. Scratching the wound can worsen the itching cycle, leading to increased inflammation and a heightened risk of scarring.
A 2013 study identified two mechanisms by which HOCl can alleviate itchiness in wounds:
- Antimicrobial Action: HOCl exhibits strong antimicrobial properties, particularly against Staphylococcus aureus, thereby helping to eliminate harmful microorganisms at the wound site.
- Anti-Inflammatory Effects: HOCl reduces the activity of histamine, leukotriene B4 (LTB4), and interleukin-2 (IL-2), contributing to decreased inflammation.
Recent investigations revealed that the application of HOCl gel effectively prevented the formation of eczematous lesions and instances of scratching. The findings indicate that HOCl directly mitigates sensory responses, leading to significant reductions in both itching and inflammation in living organisms. Notably, half of the participants in the study reported relief from itching on the first day of treatment, while a remarkable 85% experienced significant improvement in itching by the third day of HOCl treatment.
The Importance of Wound Perfusion in Healing
Oxygen is essential for collagen synthesis, the formation of new capillaries, and infection control. The perfusion and oxygenation of tissues are closely linked, significantly impacting wound healing. A study conducted by Bongiovanni investigated the effects of topical hypochlorous acid (HOCl) on venous leg ulcers. The research team measured the oxygen supply to the wound and found a significant increase in oxygen pressure in the surrounding skin tissues of patients treated with HOCl, observed just 15 to 30 seconds after application. This elevated oxygen level remained consistently high for approximately 72 hours post-treatment. Furthermore, all venous ulcers treated with HOCl healed completely within 2 to 5 days, with continued improvement noted up to 180 days after treatment initiation.
Effective Scar Management
Scar management is intricately linked to every phase of wound healing, involving a complex array of signaling molecules that regulate the healing process at the molecular level. The ongoing synthesis and breakdown of collagen are crucial in remodeling the wound matrix for about six months following wound formation. Among the common types of scars, hypertrophic scars (HTS) and keloid scars are particularly noteworthy.
Both keloids and hypertrophic scars share several characteristics, including post-injury growth, dry skin, and itching. Recent studies indicate that chronic inflammation in the deeper layers of the skin at the wound site influences both scar types. During normal wound healing, extracellular cytokines help regulate collagen fiber production. However, various genetic and environmental factors can disrupt this signaling, leading to an overproduction of collagen fibers, which manifests as HTS. In hypertrophic scars, collagen production occurs independently and without proper control.

In the case of keloid formation, excessive scar tissue growth continues during the later stages of wound healing, typically between 6 to 18 months post-injury. This results in uncontrolled collagen accumulation that extends beyond the original wound boundary. Timely intervention and the application of HOCl are vital for managing abnormal tissue growth and minimizing scar formation.


Patient with itchy hypertrophic scar on left arm after surgery. After 8 weeks of HOCL treatment, scar height and itching were significantly reduced.
The Benefits of Combining HOCl and Silicone for Scar Management
The effectiveness of combining hypochlorous acid (HOCl) and silicone in treating hypertrophic scars (HTS) and keloids, as well as alleviating associated itching and pain, has been explored due to HOCl’s positive effects on all three stages of wound healing at both the cellular and molecular levels. Recognized for its antiseptic properties, HOCl is considered safe and effective for use on skin and scars. Silicone has a long-standing reputation in scar treatment, making this combination particularly promising.
One notable advantage of a hybrid gel that combines silicone and HOCl is its ability to be applied directly to the wound site after surgery, setting it apart from many other silicone-based products. This innovative treatment approach facilitates rapid inflammation reduction, disinfection, and control of scar formation.
A double-blind study revealed that the HOCl/silicone hybrid gel significantly improved pain, itching, elasticity, and scar height in patients with HTS or keloids compared to a 100% silicone topical agent. These findings suggest that the combination of HOCl and silicone could have a more substantial impact on scar prevention and management.
HOCl is highly recommended throughout all stages of surgery, including procedures like injections and laser treatments. Before surgery, it is advisable to remove excess facial makeup and apply a spray of HOCl to the surgical site. Post-operation, HOCl remains crucial for preventing infection and promoting optimal recovery over an extended period.
Conclusion: The Future of Wound and Scar Treatment
As research continues to unveil the extensive benefits of hypochlorous acid, its position as the gold standard for wound and scar treatment is solidifying. With its potent antimicrobial and anti-inflammatory properties, HOCl represents a powerful tool in modern medicine. Healthcare professionals are encouraged to consider HOCl in their treatment protocols, offering patients a safer, more effective option for managing wounds and minimizing scar formation.
In summary, hypochlorous acid is not just a treatment—it’s a transformative approach to wound care that holds the potential to change the lives of countless patients worldwide. With its proven efficacy, HOCl is poised to set new benchmarks in the healthcare industry, ensuring quicker recoveries and improved outcomes for those in need.